Ideas can really take on a life of their own. And like any other living thing, they require proper nourishment and a suitable environment in which to flourish. Same as how certain creatures grow relative to their surroundings, so too do ideas need room to reach their full potential. Such are the minds at The Sener Laboratory.
For nearly 12 years, Dr. Alp Sener, Chair and Chief of Urology at London Health Sciences Centre, has been asking himself: how can we improve organ function for transplant patients? Today, once an organ is harvested, it’s flushed with a solution and stored in a fridge for up to two days. But the more time passes, the more damage an organ sustains. Some organs, such as the kidneys, can even take a while before becoming fully functional again.
“It's like the kidney is almost stunned. We call it a sleepy kidney,” explains Dr. Sener. His enthusiasm is contagious. You can tell he’s building to something.
To address problems affecting transplant organs, Dr. Sener began looking into hydrogen sulfide. As part of a three-molecule family which includes nitric oxide and carbon monoxide, hydrogen sulfide, like the others, is a poisonous gas. Only it’s a gas our bodies produce naturally as a sort of protection.
This led him to consider hibernation. As an animal’s temperature, breathing and heart rate slow down upon entering hibernation, hydrogen sulfide levels in the blood go up. Studies have also shown how hibernating animals can’t survive when hydrogen sulfide production is blocked, whereas increasing it can induce a state of hibernation. Similar to how an organ’s metabolic rate drops and is deprived of oxygen when cooled, Dr. Sener remembers it sounded an awful lot like what organs go through when placed in a cooler prior to transplant.
Experiments confirmed transplant organs flushed with standard preservation solution combined with hydrogen sulfide outperformed the standard solution on its own. However, hydrogen sulfide donor molecules, such as those used in the initial animal experiments, weren’t approved for human testing. The team soon came across sodium thiosulfate, a similar compound readily available to clinicians.
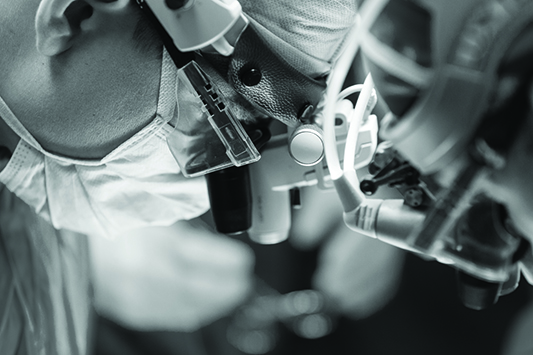
After several more years of testing and making the necessary adjustments to the dosage, Dr. Sener and his team were delighted to find similar results using sodium thiosulfate. And on March 21, 2021, Dr. Sener performed the world’s first human transplant using this new preservation method.
“The day following transplant, our patient was making urine. This was remarkable as she normally made no urine while on dialysis. It’s very exciting,” Dr. Sener exclaims. He hopes replicating this success will encourage transplant programs across Canada to participate in multicentre studies—all of which will require more funding.
Dr. Sener considers himself incredibly fortunate because without donor support, vital research such as this would not be possible. Already, recent events have garnered some attention, spurring his investigation onward with optimism. And working alongside a team driven by innovation and improving patient care, Dr. Sener is cultivating an environment wherein ideas thrive, research inspires and people go on to live healthier, more fulfilling lives.
